How to Build a Successful Referral Program for Your Medical Practice
A strong referral program isn’t just a marketing tactic—it’s a strategic bridge between doctors and the patients who need them most. In today’s hyper-competitive, attention-deficient healthcare landscape, traditional advertising often fails to cut through the noise. But one thing still moves people to act: trust. Whether it’s a patient referring a friend or a provider recommending your practice, that trust carries more weight than any ad spend.
For small to mid-sized private practices, building a referral network can mean the difference between simply surviving and sustainably growing with the right patients—the ones your practice is most equipped to help. This guide breaks down how to create a referral system that’s ethical, effective, and built for the long haul.
Why Referral Programs Matter More Than Ever
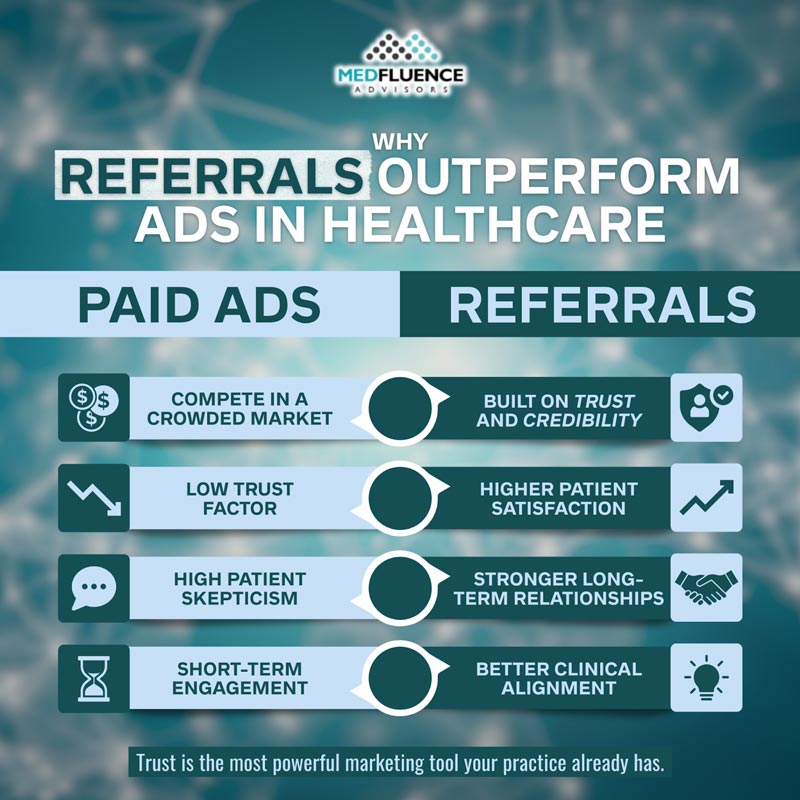
Let’s be honest: most private practices don’t have the time, budget, or interest to compete with hospital systems and corporate clinics in the digital ad arms race. But there’s one area where independent providers still have the upper hand—relationships. When patients or referring providers trust you, they don’t need convincing. That’s why referral programs aren’t just a nice-to-have—they’re one of the most reliable ways to attract patients who are actually a fit for your services.
The problem? Most small and mid-sized practices are stuck trying to patch together inconsistent word-of-mouth or rely on outdated directories. Meanwhile, they’re losing patients to louder—but not necessarily better—competitors.
Patients today are overwhelmed with choices, but they’re also skeptical. A friend’s recommendation or a provider’s trusted handoff cuts through that noise. And it’s not just anecdotal—data consistently shows that referred patients tend to have higher satisfaction rates, better follow-through, and stronger clinical engagement. They show up ready to act, not just “see what their options are.”
Some of the most successful practices we’ve worked with don’t spend tens of thousands on ads. Instead, they build intentional, systematized referral pipelines—both from other providers and from patients themselves. These aren’t random one-off mentions. They’re supported by workflows, follow-up, and consistent relationship building.
There’s a clear distinction between passive referrals (“Hey, someone told me about you”) and proactive ones (“My doctor said you’re the best person to help with this”). The latter happens when you intentionally build and maintain referral pathways—not just hope for the best.
The good news? Creating a reliable referral engine doesn’t require a big marketing budget or a full-time outreach team. But it does require structure, clarity, and a repeatable process. And it starts by knowing exactly who you’re trying to reach.
Setting the Foundation: Define the Patients You Want to Attract
The fastest way to stall a referral program is by casting too wide a net. Not every patient is the right fit for your practice—and not every referrer knows that unless you make it crystal clear. A strong referral system starts with defining exactly who you’re built to help.
Many practices chase volume, thinking more leads will solve their growth problem. In reality:
- More isn’t better if the patients aren’t a clinical match
- Clarity beats quantity when it comes to referrals
- Referrers want guidance—they’re not going to guess who you want
Start by mapping out your ideal patient profile. Ask yourself:
- What conditions do you treat most effectively?
- What goals do your best-fit patients have—relief, clarity, long-term care?
- What’s their mindset—are they frustrated by misdiagnoses, tired of short-term fixes, open to innovative procedures?
- What’s their story—undiagnosed symptoms, bouncing between specialists, skeptical of “quick fixes”?
Once you have that clarity, identify the providers who see those patients first. Strong referral sources might include:
- Primary care physicians noticing chronic issues that aren’t improving
- Therapists or mental health professionals seeing physical symptoms tied to emotional stress
- Chiropractors or PTs treating pain that hasn’t responded to their modality
- Naturopaths or wellness providers whose patients are seeking evidence-backed alternatives
Then, arm those referrers with clear, useful messaging:
- Create a one-pager or intro email with your treatment focus, ideal patient traits, and next steps
- Emphasize what makes your approach different—especially if it fills a gap in traditional care
- Spell out who isn’t a match for your practice (e.g., certain conditions, insurance types, or health beliefs)
This level of precision helps:
- Prevent wasted referrals that go nowhere
- Reduce intake bottlenecks and misaligned expectations
- Make it easier for the right patients to find the right care—yours
Dial in your messaging, and you’ll stop attracting “maybe” patients—and start hearing, “I’ve been looking for this for months.”
Building Relationships with Like-Minded Providers
Referral relationships with other providers aren’t built on email blasts or generic handouts. They’re built on trust—and that takes clarity, consistency, and a genuine desire to collaborate. The goal isn’t just to get referrals. It’s to connect with providers who share your mindset: solving real problems for patients who often fall through the cracks.
Here’s how to build strong, referral-worthy partnerships:
-
Establish Mutual Trust with Referring Providers
You’re not just asking for patients—you’re asking another provider to stake their reputation on you. That means:
- Be upfront about what you do—and what you don’t. Precision builds credibility.
- Share clinical outcomes or case examples (anonymized, of course) that show how you help patients they likely struggle to treat.
- Make their job easier. Don’t add friction to their already-busy workflow.
-
Start the Conversation Without Sounding Transactional
No one likes being “sold to.” Your outreach should feel like the beginning of a shared solution, not a pitch. You can:
- Lead with a shared patient problem (e.g., “We’ve both seen patients with chronic sinus symptoms who bounce between ENT and PCP with no clear answer.”)
- Ask about their experience with those cases, then explain how your approach fills the gap.
- Frame it as clinical collaboration, not competition or solicitation.
-
Make Referring Easy and Fast
If referring to you requires six steps or a clunky fax form, most providers won’t bother. Streamline it by offering:
- Clear referral instructions (digital and paper options)
- A designated referral contact—one person they can always reach
- Quick turnaround on scheduling for referred patients
- Status updates without micromanagement
-
Keep Them in the Loop—Without Crossing HIPAA Lines
Staying connected after the referral helps reinforce trust—but you have to respect privacy boundaries. Here’s how:
- Send a follow-up confirming the patient was seen, with a quick note (e.g., “John was evaluated this week—thanks for sending him our way.”)
- With patient consent, share key outcomes or treatment decisions.
- Invite feedback on the referral process—was it smooth, confusing, delayed?
Bottom line: referring providers want to know their patients are in good hands. When you make the process easy and transparent, you don’t have to chase referrals—they’ll keep coming.
Activating Happy Patients as Referral Advocates

You don’t need a massive ad budget if you’ve got satisfied patients who are willing to talk. The best referral source might already be sitting in your waiting room—it’s just a matter of timing, messaging, and making it feel natural.
-
Timing Matters: Know When to Ask
You’ll get better results if you ask at the right moment, not just whenever it crosses your mind. Aim to ask when:
- They’ve just had a positive outcome or “aha” moment
- They express gratitude or relief—that’s your window
- Their problem is finally solved or significantly improved
-
Keep the Language Natural—Not Salesy
Patients aren’t referral agents. You’re not writing a script—they’re sharing a story. Try:
- “We’re always looking to help others going through what you went through. If someone comes to mind, feel free to send them our way.”
- “If you know anyone struggling with the same thing, we’d love to help them too.”
- Keep it casual. No pressure, no jargon.
-
Create “Referral Moments”
Make it easy for patients to share their experience with others:
- Send a follow-up thank-you email with a quick prompt like, “Know someone who’s still struggling with [X]? Here’s how to refer.”
- Offer a simple testimonial form or review request right after a good appointment
- Encourage social sharing when appropriate: “We’re on Instagram/Facebook if you’d like to tag us or share your story.”
-
Use Incentives Carefully—and Legally
Referral incentives can backfire if they’re not done carefully. Consider:
- Avoiding cash or financial rewards—they often violate state and federal laws
- Using thank-you gifts that are low-cost, general (e.g., coffee cards), and not tied to medical services
- Prioritizing appreciation over promotion—patients should refer because they trust you, not because they’re getting something in return
Happy patients are your most credible advocates. Give them a reason—and a way—to talk about you, and they will.
Making Your Referral Process Frictionless
Most practices don’t have a referral problem—they have a follow-through problem. Someone hears about you, wants to refer, maybe even tries… and then nothing happens. The gap between intent and action is where referrals quietly die.
Here’s how to spot—and fix—those hidden drop-off points:
-
Identify Common Referral Bottlenecks
These are the most common places where referrals go to waste:
- Unclear referral instructions (“Do I email someone? Fill out a form?”)
- Long response times that leave patients in limbo
- No designated point of contact—referrers or patients aren’t sure who to follow up with
- Front desk breakdowns (missed calls, vague intake questions, clunky scheduling)
-
Use Simple Systems to Track and Follow Up
You don’t need a full-blown tech stack—just a system that does these three things:
- Captures how each new patient heard about you (referrer, patient name, or channel)
- Flags high-quality referrers so you can nurture those relationships
- Follows up with referred patients within 24–48 hours—ideally same-day
Bonus tip: use internal tags like “Provider Referral,” “Patient Referral,” or “Self-Referral” to track trends without creating noise.
-
Optimize Handoffs from Start to Finish
From the moment a referral is made to the patient’s first appointment, the process should feel smooth and consistent. That means:
- Phone scripts that clearly walk patients through what to expect
- Follow-up emails or texts confirming appointments and providing helpful info
- A clear “what’s next” after each touchpoint so nobody feels left hanging
-
Measure the Right Metrics
Don’t just count how many referrals you’re getting—dig deeper:
- Which sources consistently send aligned patients?
- What’s the show rate for referred patients vs. cold leads?
- Are these patients converting into long-term relationships or dropping off?
When you smooth out the rough edges, referrals don’t just increase—they start working better.
Using Tech to Keep It Simple and Scalable

You don’t need to turn your practice into a software company just to manage referrals. The right tech tools can help you streamline, track, and grow—without overwhelming your team or creating more busywork.
Here’s how to use technology to support (not complicate) your referral process:
-
Choose Referral Tracking Tools That Actually Get Used
Start with tools that are easy for your front desk, clinical team, and referrers to use. That might mean:
- A shared Google Sheet or simple CRM for tracking referral sources
- Automated email sequences for referred patients
- Form fills or intake portals that referrers can complete in under 2 minutes
Avoid tools that require extensive training or manual data entry. If your staff avoids it, it’s already a fail.
-
Integrate the Tools You Already Use
You don’t need to reinvent the wheel—just make your existing systems work together. Look for ways to connect:
- EMRs (electronic medical records) with basic patient source tracking
- CRMs or intake software with scheduling tools like Calendly or Klara
- Patient communication platforms (email, SMS, voice) with referral alerts or automations
The goal is simple: one handoff, one system, no confusion.
-
Add Automation—But Keep It Human
Automation should enhance the patient and referrer experience, not replace it. Consider automating:
- Appointment reminders for referred patients
- Referral acknowledgment emails (“Thanks for the referral—we’ll keep you in the loop!”)
- Feedback requests to keep your process improving
But skip the robotic tone. Personalize wherever you can, even if it’s just a quick first-name insert and a thank-you line.
-
Don’t Overdo It
Tech is great—until it creates more problems than it solves. Watch for signs of overengineering:
- You’re using five different platforms and no one knows which one to check
- Referrers or patients complain about too many steps or emails
- Your staff is spending more time on the tool than on the patient
Remember: the best tech supports relationships. It doesn’t replace them.
Keeping Referrers Engaged Long-Term
Getting a referral once is great. Getting consistent referrals from the same provider? That’s practice growth. But that only happens if you stay relevant, reliable, and easy to work with—without overdoing it.
Here’s how to keep the momentum going:
-
Don’t Treat Referrals Like One-Off Wins
- A single referral isn’t a relationship—it’s a test.
- You prove your value through how you follow up, communicate, and support the patient they sent.
-
Follow Up Without Being a Nuisance
- Referrers don’t want daily updates—they just want to know the handoff didn’t vanish into a black hole.
- Send brief updates after the first visit or resolution (with patient consent). A simple “Thanks again for sending [Patient], here’s where we’re at” goes a long way.
-
Create Value Between Referrals
- Host quarterly case reviews, short virtual check-ins, or informal meetups to stay connected.
- Send them useful, clinically relevant info that shows you’re thinking beyond “send us patients.”
-
Stay Top-of-Mind Without Constantly Asking
- A quick email with a clinical success story, shared blog post, or even just a “Let us know if you need anything” keeps the door open.
- Make it easy for them to refer again—no hunting for forms or contacts.
Consistent, respectful contact keeps your practice at the front of their mind—without becoming background noise.
Troubleshooting: What to Do When Your Referral Program Stalls
Even the best-designed referral programs hit a wall. If your numbers are dropping—or worse, flatlining—it’s time to investigate before the damage snowballs.
Start here:
-
Spot the Bottlenecks
- Where are referrals falling off? Common culprits:
- Referral forms that are too complicated
- No follow-up after a patient is referred
- Poor handoffs at the front desk
- Delays in scheduling
- Talk to your team—and a few referrers—to identify where things are getting stuck.
- Where are referrals falling off? Common culprits:
-
Avoid These Common Mistakes
-
- Asking too soon: If a provider barely knows what you do, they’re not ready to refer.
- Asking the wrong people: Not every provider sees the patients you treat.
- Unclear messaging: If your value proposition is muddy, no one knows why they should send patients your way.
-
-
Realign with Your Practice Goals
- Are you attracting the right patients—or just anyone?
- Do your referral sources align with your best outcomes?
- Is your team trained to handle new leads with clarity and consistency?
Sometimes a stalled program just needs a few tweaks—a better email template, clearer referral instructions, or a quick lunch with a high-potential provider.
But don’t wait. If things slow down, treat it like you would with a patient: investigate, diagnose, and adjust before it turns into something worse.
Referral Growth That Doesn’t Feel Like Marketing

The strongest referral programs don’t rely on charm, luck, or pushy tactics. They run on clarity, consistency, and mutual benefit—for providers and patients alike. When done right, a referral program doesn’t feel like “marketing.” It feels like what healthcare should be: people connecting each other to the help they need, when they need it.
And while you can build much of this yourself, it’s also worth considering tools and strategies that keep your system tight without overcomplicating it. That’s where something like Medfluence comes in—not as another software platform to wrangle, but as a partner in helping you simplify, track, and improve what’s already working. No silver bullets, no magic dashboards—just support that helps your practice grow on its own terms.
Referral success doesn’t come from asking more people, more often. It comes from asking the right people, at the right time, in a way that feels honest and useful. With the right systems in place, referrals stop being something you hope for—and start becoming something you can count on.


